Knowing details of outstanding claims filed to insurance carriers (payers) is vital to any medical practice. DuxWare’s Dunning Report displays outstanding claims grouped by payer. It facilitates better collection practices by allowing the user to assess the balance information and make one call to the payer to solve many outstanding balance issues.
This vital report can also expose issues such as
- sequencing errors that could be prohibiting a claim from being filed through your clearinghouse
- claims that have not been transferred to the next responsible party
- filing a claim to the incorrect payer.
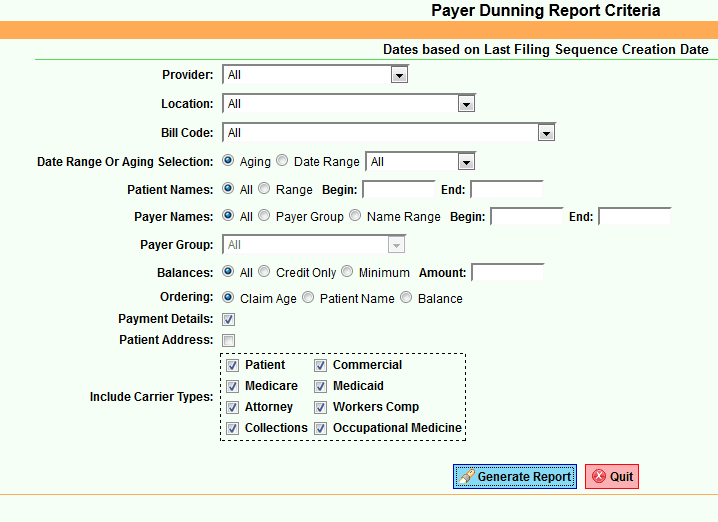
This interactive report can be filtered by
- Physician
- Location
- Claim Aging
- Patient Names
- Payer
- Payer Group
- Minimum Balance
- Credit Balances
Ordered by
- Claim Age,
- Patient Name
- Balance Amount
Report output can also be filtered to include or exclude payer types. Data is formatted on the report in such a way that users can work directly from the report.
Report data includes
- Claim Number
- Patient Name
- Account Number
- Date of Birth
- Phone Number
- Social Security Number
- Policy and/or Group Number
- Claim Date
- Physician
- Location
Also included are line-item details for each claim including the Total Claim Balance and Claim Age.
Any attached Billing Messages are also included with the claim. All Claims are grouped on the report under the associated Payer.
- The Payer Name
- Telephone Number
- Payer Address
- Total Outstanding for the Payer
Reviewing and working DuxWare’s Dunning Report on a routine basis can result in a very clean Accounts Receivable for your practice and eliminate claims from falling through the cracks. Unfortunately, getting your claims to their respective payers is only half the battle. Follow-up of outstanding claims is key to managing your Accounts Receivable successfully. Most practices will run and work the Dunning Report on a 30-day or bi-weekly regimen just after posting their last round of remittances.